Abstract
The methodologies of acupuncture trials for Parkinson Disease have been inconsistent, with variations in point selection. This critical literature review (CLR) evaluates the methodologies of acupuncture trials, determining the efficacy of acupuncture points in alleviating motor related symptoms of PD and whether sham acupuncture is effective as a control to mitigate the placebo effect. Databases were searched for trials between 2005 and 2020. A qualitative assessment of the methodology was applied, and a quantitative evaluation of the acupuncture points used in the trials; using the P-values of each study to determine the average P-value. Only two trials used an adequate control to mitigate against the placebo effect. And acupuncture points such as Tai Chong (Liv 3) had a lower average P-value than other points. However, this CLR found that although different acupuncture points had lower average P-values, to infer higher efficacy is problematic due biases, heterogeneity, and small sample sizes of the trials.
1. Introduction
Parkinson’s disease (PD) is a progressive neurodegenerative illness leading to the death of dopamine-containing brain cells (Alexander, 2004). The estimated total cases of people in the UK suffering from PD in 2018 was 145,519, about 1 in every 450 people (Parkinsons UK, 2018).
The pathogenesis of PD involves the accumulation of the alpha-synuclein protein; these aggregations of proteins are called Lewy bodies (Ariadna and Benjamin, 2014). The degeneration and depigmentation of dopaminergic neurons in the substantia nigra, part of the basal ganglia; causes biochemical changes in the corpus striatum (Ramsden, Parsons, Waring and Ho, 2001). The increase in the neurotransmitter acetylcholine compensates for the decrease in dopamine; this imbalance between dopamine and acetylcholine leads to the characteristic motor dysfunction associated with PD (Aosaki et al., 2010). The most prominent of these are trembling, stiffness of limbs, impaired balance and coordination, postural instability, shuffling gait, and slowness of movement (bradykinesia) (Alexander, 2004; Thanvi and Lo, 2003). Non-motor related symptoms can arise too, such as depression, sleep disorders, fatigue, and dementia (Parkinsons UK, 2018).
Qualifying the pathogenesis of PD is not universally standardised and there are different scales of PD, with Unified Parkinson’s Disease Rating Scale (UPDRS) being the most widespread for evaluating the efficacy of interventions in clinical trials (Lee and Lim, 2017). The UPDRS was recently revised and enhanced by the Movement Society Disorder, to form the composite MDS-UPDRS acronym (Goetz et al., 2008). This paper will be evaluating only the motor related symptoms of PD, therefore only the data of the trials subsumed under the UPDRS II and UPDRS III are applicable. The UPDRS II is a self-evaluation of the severity of motor related symptoms in daily life such as handwriting, eating or getting dressed, with a scale of 0 (normal) to 4 (severe) (Goetz et al., 2008). UPDRS III is a clinical assessment of the patient by an assessor using the same scale as UPDRS II on categories such as gait, tremor, or leg agility (Goetz et al., 2008).
PD is considered idiopathic, though genes and lifestyle have been linked as an aetiological feature (Sidransky and Lopez, 2014; Ramsden, Parsons, Waring and Ho, 2001). Currently, there is no cure for PD, and the symptoms are managed through drugs such as Levodopa, dopamine agonists (activates dopamine receptors in the brain) and more rarely, anticholinergic drugs (blocks the neurotransmitter acetylcholine to help with tremors) (Varanese et al., 2011). However, there are adverse side effects which include nausea, tiredness, loss of appetite, vomiting and dyskinesias (spontaneous, involuntary movements) (Parkinson’s Disease Foundation, 2018). Moreover, with extended use of these drugs, there is a gradual loss of efficacy as well as dyskinesia (tremoring) and further complications which can be worse than the symptoms of PD itself (Thanvi and Lo, 2003). Therefore, managing the symptoms of PD using medication alone can be distressing and challenging as the disease progresses. This has led to patients exploring complementary therapies such as acupuncture as an adjunct to Western medication (Ferry, Johnson, and Wallis, 2002). Acupuncture is becoming an increasingly popular complementary therapy for patients with PD (Lee and Lim, 2017). Previously, its efficacy was backed only through limited and anecdotal evidence with clinical trials often failing to meet rigorously designed randomized controlled trials (RCTs). However, the standard in methodology has increased in recent years (Fan et al., 2018), and there is a growing body of evidence suggesting acupuncture may be helpful in alleviating the motor and non-motor related symptoms associated with PD (Were, 2018).
Within the Chinese classical texts, commentators have argued that there are references suggestive that the Chinese classics were referring to PD dating back to 425 BC (Dong, Zhang and Román, 2006). However, it is difficult to prove that they were describing a patient with PD, as the symptoms are so variable (NHS, 2016). Moreover, PD is a heterogeneous disease with a complex pathology, and it is not always easy to classify even within Western Medicine (Stoker and Greenland, 2018). This can lead to misdiagnosis as there is no diagnostic test available and the symptoms of PD imitate other diseases (Parkinsons UK, 2018). Furthermore, the diagnosis of PD is often only confirmed when the symptoms respond to drugs such as Levodopa (Suchowersky et al., 2006).
The motor related symptoms of PD, such as involuntary shaking of parts of the body (tremors) (NHS, 2016) are characterized according the Su Wen as Wind “[causing] swaying and dizziness, without exception they are associated with the liver” (Unschuld, 2011;626). This has led modern commentators to state that Liver Wind is the most likely pathological condition that describes PD, as tremoring of the sinews is always associated with Internal Wind and controlled by the Liver (Maciocia, 2008). Liver Wind, synonymous with Internal Wind, causes involuntary movements as well as paralysis and rigidity too (Maciocia, 2015), mirroring some of the motor related symptoms of PD. The aetiology of Liver Wind arises mainly from long-standing Liver and Kidney Yin Deficiency (Stephenson, 2017; Maciocia, 2008). Deficiencies of Yin develop naturally in the aging process (Dashtar et al., 2016), correlating with PD being a disease that affects people in their later years of life, with one meta-analysis study showing the mean age of people with PD was 61.2 years (Pagano et al., 2016).
swaying and dizziness, without exception they are associated with the liver” (Unschuld, 2011;626). This has led modern commentators to state that Liver Wind is the most likely pathological condition that describes PD, as tremoring of the sinews is always associated with Internal Wind and controlled by the Liver (Maciocia, 2008). Liver Wind, synonymous with Internal Wind, causes involuntary movements as well as paralysis and rigidity too (Maciocia, 2015), mirroring some of the motor related symptoms of PD. The aetiology of Liver Wind arises mainly from long-standing Liver and Kidney Yin Deficiency (Stephenson, 2017; Maciocia, 2008). Deficiencies of Yin develop naturally in the aging process (Dashtar et al., 2016), correlating with PD being a disease that affects people in their later years of life, with one meta-analysis study showing the mean age of people with PD was 61.2 years (Pagano et al., 2016).
Table 1 – Underlying Patterns of Liver-Wind – (Maciocia, 2008)
| Full Conditions | Empty/Deficient Conditions |
| Liver-Yang Rising | Liver-Blood |
| Phlegm-Heat | Liver-Yin |
| Liver-Fire | Kidney-Yin |
Liver-Wind arises from different underlying patterns in Chinese Medicine (CM) (See Table 1). Therefore, patients suffering with PD, may be diagnosed within the CM paradigm as having one of these underlying conditions, with different acupuncture point configurations treating those conditions rather than using a generic standardised approach for the more generalised concept of PD (Maciocia, 2008). Empty conditions have the characteristic of allowing Liver Wind to occupy the empty space and cause tremoring (Maciocia, 2008). Whereas Full conditions, such as Phlegm can prevent the acupuncture channels from being nourished by Blood and Fluids, drying the sinews, and causing an invasion of Internal Wind (Maciocia, 2008).
In a meta-analysis, Lee and Lim, (2017) found that a total of 65 different acupuncture points was used across the trials cross-sectioned for treating PD. The acupuncture point most used was Tai chong (Liv 3), but it had only been used 11 times out of the 25 trials evaluated. When treating just Internal Wind, there are general acupuncture points prescribed to extinguish it. Maciocia (2008) gives the following points for extinguishing Wind (See Table 2). Yang ling quan (GB 34) and Tai chong Liv 3 were the only acupuncture points recommended by Maciocia (2008) amongst the 65 acupuncture points that were used from the meta-analysis conducted by Lee and Lim, (2017). This highlights the divergences in opinion within the acupuncture community as to the most conducive treatment plan in treating symptoms of PD.
Table 2 – Acupuncture points for treating Liver-Wind – Maciocia (2008)
General Points | Local points – Arm | Local points – Leg |
GB-20 (Feng chi) | LI-11 (Qu chi) | St-31 (Bi guan) |
LI-11 (Qu chi) | LI-10 (Shou san li) | GB-31 (Feng shi) |
TH-5 (Wai guan) | TH-5 (Wai guan) | St-36 (Zu san li) |
GB-34 (Yang ling quan) | LI-4 (He gu) | GB 34 (Yang ling quan) |
Liv-3 (Tai chong) | Ht-7 (Shen men) | St-41 (Jie xi) |
Du-16 (Feng fu) | GB-40 (Qiu xu) | |
Ki-3 (Tai xi) | ||
Sp-6 (San yin jiao) |
However, acupuncture point selection in these trials was not arbitrary and there are guidelines such as, Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) (Altman et al, 2010) to help clarify the style of acupuncture and the rationale behind point selection. However, this lack of standardisation and consistency in point selection for treating symptoms of PD undermines any substantiated conclusions that could be drawn from the results. Through accumulating data on the efficacy of acupuncture points, a more standardised configuration may become evident. Currently, there has been little comprehensive research into the methodology of acupuncture point selection when treating patients with motor related symptoms of PD. Previous critical literature reviews (CLR) focused on whether acupuncture can alleviate any or some of the symptoms of PD (Were, 2018). Whilst these studies have lent support to the efficacy of acupuncture in treating PD, there has not been an extensive examination on the methodology of point selection to date.
The methodology of acupuncture trials can be extended to the aspect of blinding, with some forms of sham acupuncture shown to have similar nonspecific effects in treating PD symptoms as real acupuncture (Kluger et al, 2016). The placebo effect is well documented within PD control trials. The strength of belief in symptom improvement has been shown to be directly involved in the dopaminergic pathways and having a powerful effect on the brain’s neurochemistry, releasing dopamine into the striatum (Lidstone, Schulzer, Dinelle et al., 2010; De la Fuente-Fernandez and Stoessl, 2002). Sham acupuncture can take various forms; pressing a blunt needle on the skin, placing the needle in an incorrectly designated area, or creating a ‘phantom acupuncture’ effect with visual aids (Lee et al., 2014). That certain forms of sham acupuncture can have similar results to real acupuncture is not surprising given that just pressing acupuncture points results in a physiological reaction (Matsubara et al., 2011). However, without an adequate control that mitigates the placebo effect, patient expectations on the outcomes of treatment may obscure the quality of the results (Linde et al, 2007).
The aim of this CLR will be to evaluate primary research papers, published within the last fifteen years, on the efficacy of acupuncture in alleviating motor related symptoms for patients with PD and the rationale for different acupuncture points. Moreover, it will examine some of the other methodological shortcomings of recent acupuncture trials, such as sham acupuncture. Lastly, this paper will briefly examine whether a standardised point selection is warranted for future RCT or whether a more individualised approach is more appropriate for acupuncture trials (MacDonald, 2019). A CLR is the most favourable method to address the question as it will enable a collation of relevant clinical trial papers since 2005 and evaluate their methodology, giving readers an overview and analysis of the different point selection for treating motor related symptoms of PD.
2. Method
The search criteria of published primary research since 2005 was used to determine the efficacy of acupuncture points in treating motor related symptoms of PD. The search of databases included Google Scholar, PUBMED, Greenwich University E-Library, Science Direct, Wiley Online library, Cochrane Library and Trip Database (See appendix 1). Keyword terms included ‘acupuncture’ AND ‘Parkinson’s or Parkinson’s disease employed ‘IN TITLE’. The European Journal of Oriental Medicine (EJOM) and The Journal of Chinese Medicine (JCM) were also searched for relevant journals. Clinical Studies were included if all the following criteria were met:
Table 3 – Inclusion Criteria
Published papers within the last 15 years and published or translated into English
Human trials only
Only published material
Motor related symptoms of PD reported
Only primary data and research, discounting meta-analysis papers and systematic studies
Real acupuncture, electro-acupuncture, and scalp acupuncture
Full text of an article, discounting abstracts to decrease bias
Sample population must be more than ten participants
Table 4 Exclusion Criteria
Acupressure trials
Evidence produced pre-2005
Unpublished papers
Non-English research papers
Non-motor related symptoms of PD such as depression or anxiety
To avoid the risk of bias, the Cochrane’s checklist was applied to each study (See Appendix 4) that meets the inclusion criteria. The checklist looked at the five domains of selection, performance, attrition, reporting and other biases within each trial. The trials were also appraised using the STRICTA (See Appendix 3) and CASP Randomised Controlled Trial Checklist (See Appendix 2) to determine their methodological strengths and weaknesses.
The average P-value will be only calculated when the acupuncture point was used in at least two studies and only for UPDRS II and UPDRS III. P-values for individual measurements, primary or secondary, of gait, stride and cadence were not be included for consistency and to avoid selective reporting bias or p-hacking (Vidgen and Yasseri, 2016). The P-value is the most valuable calculation as it takes into account the sample size and data variability to determine whether the null hypothesis should be rejected, and whether a statistical difference can be found between the control and experimental group. Combining P-values is a precise method using formulas such as the weighted Z‐method or Fisher’s test (Whitlock, 2005). However, due to the lack of the required data from these trials, it is not possible to formulate these calculations. Therefore, a more simplified method of combining the P-values was devised; adding the total number of P-values and dividing by the number of studies to get an average. This may give an indication of which points might carry more efficacy in treating the motor related symptoms of PD.
3. Results
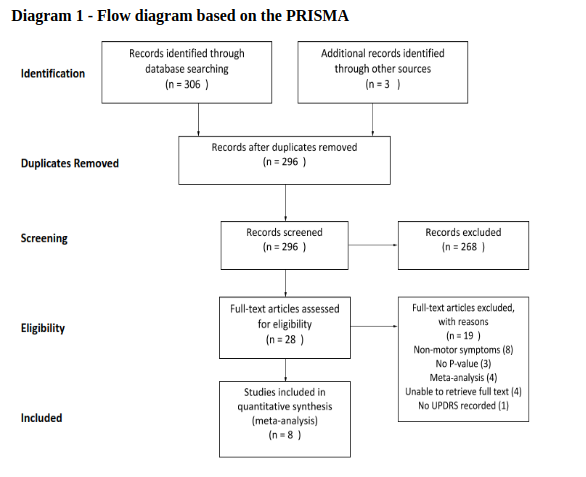
The search of the online databases found 306 articles, plus 3 articles from a library hand search (see Appendix 1). After duplicates were removed and the screening process finalised, 28 articles were further evaluated within the parameters of the inclusion and exclusion criteria. After these criteria were applied, 8 studies were found to be eligible for the CLR (see diagram 1) and summarized in Table 5.
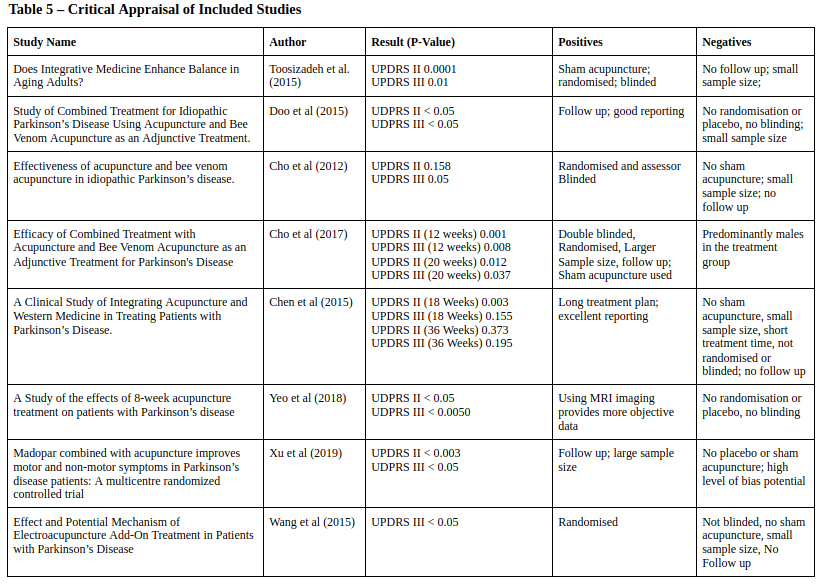
Generally, all studies adhered to the STRICTA guidelines (See appendix 3). Studies such as Toosizadeh et al (2015), Chen et al (2015), Yeo et al (2018) and Cho et al (2012) based their point selection on previous studies such as Lee (2008) or Shulman (2002). However, Yeo et al (2018) was the only study to add individualised acupuncture points, from a preselection, to the participants based on the symptoms of the patient in conjunction with Tai chong (Liv 3) and Yang ling quan (GB 34), that was given to all the participants.
Only Toosizadeh et al (2015) and Cho et al (2017), used sham acupuncture or a placebo control, the other studies used the continuation of PD medication as the control. Cho et al (2017) found that sham acupuncture initially produced statistically significant results when compared to the baseline after 12 weeks. However, the efficacy was not sustained in the sham acupuncture group when following up after 20 whereas the intervention group continued to show statistically significant improvements compared with the baseline. Toosizadeh et al (2015) also used sham acupuncture as a control by inserting the needles just under the skin, at non-acupuncture points, minimal intensity but found that there was no improvement in UPDRS II and III in the sham control group, even in the short-term.
All trials except Chen et al (2015) showed statistically significant results with the P-value below 0.05 compared to the baseline. Although many of the trials reported P-values which were statistically significant, this significance is lost by the weakness of their methodologies, with six of the studies not using a placebo or sham acupuncture, increasing the likelihood of bias.
In terms of evaluating the risk of bias based on Cochrane, only Cho et al (2017) achieved a ‘Good’ standard. The remaining studies were only ‘Fair’ or ‘Poor’ due to lack of randomisation and blinding. However, all studies assessed had a low risk of bias in terms of incomplete data outcome and selective reporting (See appendix 4).
All the studies had sample sizes under eighty participants, with three of the studies, Doo et al (2015), Toosizadeh et al (2015) and Yeo et al (2018) having sample sizes of just fifteen participants or under. Therefore, even with P-values showing statistically significant results, due to the small sample sizes there is a stronger potential for type II errors to occur (Kim, 2015).
The treatment times in the studies varied between 15 minutes and 30 minutes, with 15 minutes being the most favoured needle retention time. The number of treatment sessions varied enormously in the studies cross sectioned, varying between just 3 sessions to 72 sessions.
All the studies except Chen et al (2015) used electrical acupuncture, with a frequency of between 2 Hz – 4 Hz to get the sensation of De Qi with some studies continuing or commencing the treatment with 100 Hz – 120 Hz stimulation, an intensity just below muscle contraction.
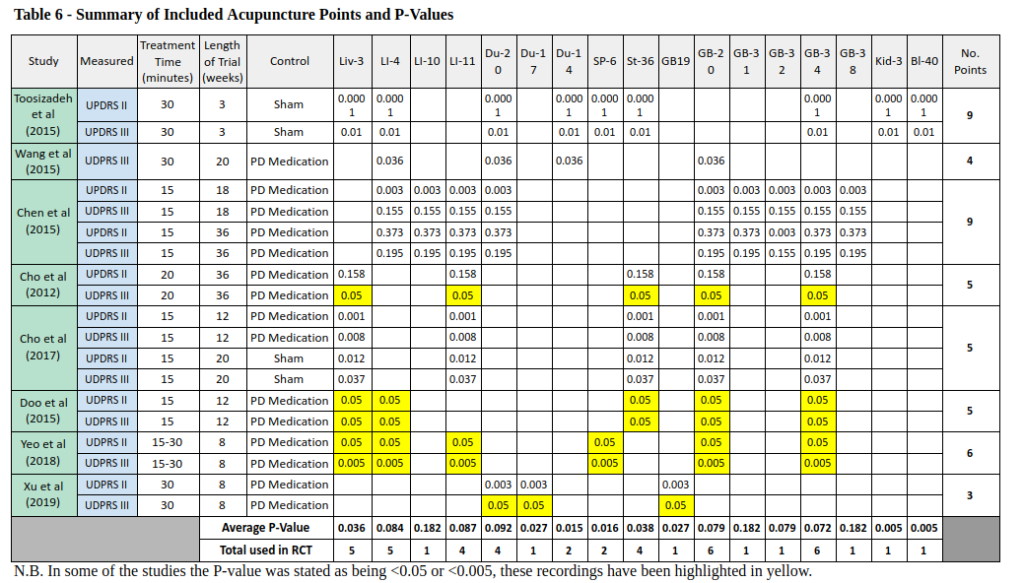
Table 7 – Average P-Value of Acupuncture Point and Frequency of Use
Acupuncture Point | Chinese Name | English Translation | Polarity | P Value | Frequency in Studies |
LI 10 | Shou San Li | Arm Three Miles | Yang | 0.182 | 1 |
Du 17 | Nao hu | Brain’s Door | Yang | 0.027 | 1 |
GB 19 | Nao kong | Brain Hollow | Yang | 0.027 | 1 |
GB 31 | Feng shi | Wind Market | Yang | 0.182 | 1 |
GB 32 | Zhong Du | Central River | Yang | 0.079 | 1 |
GB 38 | Yang fu | Yang Assistance | Yang | 0.182 | 1 |
Kid 3 | Tai Xi | Greater Stream | Yin | 0.005 | 1 |
Bl 40 | Wei zhong | Supporting Middle | Yang | 0.005 | 1 |
Du 14 | Da Zhu | Great Hammer | Yang | 0.015 | 2 |
SP 6 | San Yin Jiao | Three Yin Intersection | Yin | 0.016 | 2 |
LI 11 | Qu Chi | Pool at the Bend | Yang | 0.087 | 4 |
Du 20 | Bai Hui | Hundred Convergences | Yang | 0.092 | 4 |
St 36 | Zu san li | Leg Three Miles | Yang | 0.038 | 4 |
Liv 3 | Tai Chong | Great Rushing | Yin | 0.036 | 5 |
LI 4 | He Gu | Enclosed Valley | Yang | 0.084 | 5 |
GB 20 | Feng Chi | Wind Pool | Yang | 0.079 | 6 |
GB 34 | Yang Ling Quan | Yang Spring Hill | Yang | 0.072 | 6 |
LI 10, Du 17, GB 19, GB 31, GB 32, GB 38, Ki 3 and Bl 40 (highlighted in red) were excluded from further analysis as they were only included in one study, therefore an average could not be taken.
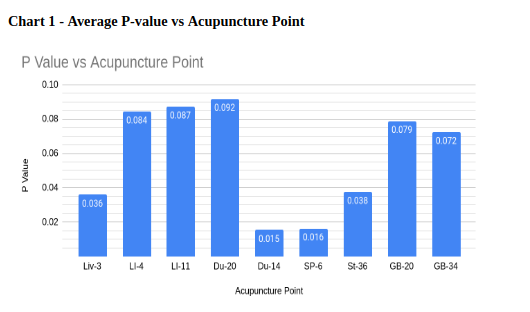
Feng chi (GB 20) and Yang ling quan (GB 34) were the most frequently used acupuncture point in the studies, used in six of the studies (see table 7). Da zhu (Du 14) and San yin jiao (Sp 6) had the lowest P-value, with an average of 0.015 and 0.016, respectively. However, they were only used in two of the studies and therefore carry less significance. The other acupuncture points that averaged a statistically significant result (P <0.05) were Tai chong (Liv 3) and Zu san li (St 36).
The majority of the studies used between four and six acupuncture points, bilaterally (see table 6). Two of the studies, Toosizadeh et al (2015) and Chen et al (2015), used 20 and 19 needle insertions, respectively, on the participants in each treatment.
4. Discussion
A recurrent issue for acupuncture trials has been minimising the risk of bias and finding an adequate control to mitigate against the placebo effect. As Lee et al (2008) pointed out, when a clinical trial is designed to be acupuncture plus PD medication versus just PD medication, it is difficult to attribute specific therapeutic effects to the acupuncture intervention. This is due to the potential influence of the placebo effect and the potential high degree of bias, from both participants and assessors. Only Toosizadeh et al (2015) and Cho et al (2017) used sham acupuncture as a control to mitigate against the placebo effect; whilst the remaining studies used just Western medication, such as Levodopa. Cho et al (2017) found that sham acupuncture showed significant differences compared to the baseline at 12 weeks. This correlates with the findings of the trial by Kluger et al (2016). After 6 weeks of acupuncture, the study found no differences between real and sham acupuncture. It concluded that acupuncture benefits the participant, but only due to the placebo effect or other nonspecific effects. Furthermore, Kluger et al (2016) references a meta-analysis he co-authored (Ghaffari and Kluger, 2014) to suggest that similar results from multiple RCTs suggest that point placement is not essential for acupuncture, real or sham, for the mechanisms of real acupuncture to work. In other words, as sham acupuncture uses incorrectly designated areas and gives the same results as real acupuncture, it does not make any difference where the needles are designated. However, Cho et al (2017) found following up eight weeks after the intervention, significant differences in UPDRS III (P-value= 0.037) and UPDRS II (P-value = 0.012) scores between the intervention group and the sham group, with the sham group’s UPDRS scores returning to baseline. This suggests that real acupuncture may have specific therapeutic effects in treating motor related symptoms of PD. However, it should be noted that this RCT used bee venom acupuncture combined with electro-acupuncture as the intervention, not just electro-acupuncture. Therefore, it would be contentious to ascribe the therapeutic effects solely to acupuncture, but it does undermine the argument that sham acupuncture and real acupuncture give the same therapeutic effects, at least in the long-term. Moreover, it lends support for sham acupuncture being a viable control to mitigate patient expectations on treatment outcomes and the placebo effect. Toosizadeh et al (2015) also found significant differences between the intervention and the control group using sham acupuncture, with the sham acupuncture group’s PD symptoms worsening. However, this trial had a small sample size, fifteen participants, and the treatment time was just three weeks with no follow up.
Sham acupuncture is a contentious issue and the ethics of exposing participants to risks without receiving any benefit in clinical trials has been questioned (Brim and Miller, 2013). The trials that used sham acupuncture, applied the needles just under the skin at non-acupuncture points (Toosizadeh et al, 2015; Cho et al, 2017) with no adverse consequences reported. However, chapter 50 of the Su Wen, warns of ‘internal harm’ if needling strays from the correct structures and can ‘cause severe injury’ (Unschuld, 2003:733). It is difficult to measure the long-term effects of sham acupuncture on participants, and to date no studies have been conducted. However, the study by Cho et al (2017) showed that sham acupuncture decreased the participants UPDRS score, lessening their PD symptoms, albeit for a short period. Conversely, Toosizadeh et al, 2015 found that the UPDRS scores increased in the control group after sham acupuncture was performed, suggesting an unfavourable risk-benefit profile for participants. However, it is difficult to ascribe this to sham acupuncture or to the degenerative effects of PD.
The rationale for acupuncture point selection for many of the studies was based on other studies and systematic reviews. Fifty percent of the studies based their point selection rationale on Lee et al (2008), even though he concluded that the case for acupuncture treating PD is ‘not convincing’. Moreover, Toosizadeh et al (2015), Chen et al (2015) and Cho et al (2012) stated that part of their rationale for point selection was based on Shulman et al (2002), even though this study concluded there was no improvement in motor related symptoms of PD (Shulman et al., 2002). And even when the studies based their rationale on the same past papers, researchers still came out with different point selection (See appendix 2).
Tai chong was used in over 60% of the studies and had an average P-value of 0.036. To use a Liver point, such as Tai chong, seems justified, as tremoring according to CM, is due to a disharmony with the Liver (Maciocia, 2008; Unschuld, 2011). Tai chong is a yuan-source and the Ling Shu recommends using these points for removing illnesses in the Yin organs, such as the Liver (Unschuld, 2016:47). Tai chong has been described by Deadman, Al-Khafaji and Baker (2016) as an essential point for ‘pacifying Liver Wind’ and can be used for excess and deficiency patterns. The Liver channel is also the only Yin channel that goes directly through the brain (Maciocia, 2006), therefore other Liver points such as Xing jian (Liv 2) might have been effective for its strong heat clearing qualities that counter Liver-Yang Rising and draining Liver-Fire, two patterns in CM that cause Internal Wind (Maciocia, 2015; Deadman, Al-Khafaji and Baker, 2016). Furthermore, the Liver channel makes up part of the Jue Yin channel, and one of the primary functions of Jue Yin is to extinguish Internal Wind (Wang and Robertson, 2008). Therefore, it is noteworthy that none of the studies used any points along the Pericardium channel that form the other half of the Jue Yin channel. Zhong chong (P 9) is a major point to extinguish interior Wind in CM (Maciocia, 2015; Deadman, Al-Khafaji and Baker, 2016) but was not used in any of the studies.
The main pathogenesis of PD is the degeneration of dopaminergic neurons, translated in CM terminology, as the decreasing of Yin. The brain is described as belonging to Yin (Unschuld, 2016) and synonymous with the Sea of Marrow (Unschuld, 2003; Maciocia, 2015) and the LingShu states that if the Sea of Marrow is deficient, “the brain revolves [vertigo], and there are noises in the ear [tinnitus]” (Unschuld, 2016:348). Tinnitus and vertigo are two of the most prominent neurotological complaints of PD (Bassetto et al., 2008) and with the brain decreasing in the amount of Marrow or Yin, the lack of Yin building points in the studies is noteworthy. Tai chong (Liv 3), Tai xi (Ki 3) and San yin jiao (SP 6) were the only Yin points used (See Table 7), equating to just 17% of the total points. If the underlying pattern of the participant was more Yin deficient and Empty rather than a Full condition such as Liver-Yang or Liver-Fire, using more Yang derived points may have had less efficacy on the symptoms than using more Yin derived points. Furthermore, it may even be detrimental to the participant if the prescription of points is based on the opposite of their underlying pattern. The importance within CM of making a distinction between Full and Empty or mixed Full-Empty patterns (See Table 1) when choosing acupuncture points cannot be overstated (Maciocia, 2015). However, some Yang points can directly and indirectly nourish the Yin, such as Bai Hai (Du 20), which was used in 50% of the studies and is used directly to nourish the sea of Marrow; and along with Da Zhu (Du 14), extinguishes Internal Wind and tonifies the Kidneys (Maciocia, 2015; Deadman, Al-Khafaji and Baker, 2016). Other noteworthy Yang points were Yang ling quan (GB 34), which helps with the smooth flow of Liver Qi and disorders of the sinews. Feng chi (GB 20) extinguishes Internal Wind, nourishes Marrow, and clears the brain (Maciocia, 2015; Deadman, Al-Khafaji and Baker, 2016). The omission of Xuan zhong (GB 39) in the trials was unexpected, given it is a major point to nourish the Marrow and treat diseases of the head and brain (Maciocia, 2015; Deadman, Al-Khafaji and Baker, 2016). Large Intestine points used were Qu chi (LI 11), a point that clears heat and drains Liver-Fire. And He gu (LI 4), a point known for its antispasmodic effect and for subduing Liver-Yang (Maciocia, 2015). Zu san li (St 36) and San yin jiao (Sp 6), are both major points to tonify Blood and Qi, and are especially useful for people with Deficiency or Empty patterns (Maciocia, 2015; Deadman, Al-Khafaji and Baker, 2016).
Point selection is complex, with differing views on the application of the 350 plus acupuncture points; with a myriad of various combinations and factors involved in the decision-making process. Factors involved in point selection can involve the current season, month, hour of treatment and even the date of birth of the participant (Van Kervel, 2012; Golding, 2008). Acupuncture, therefore, does not lend itself well to standardisation as can be illustrated from the variations of points used by the trials for the same illness. It is conceivable that the reason for the variations in point selection amongst the trials were based on the prevailing CM patterns that most participants were displaying, though this was not reported in the trials.
The prescription of different acupuncture points in treating diseases classified in Western terminology are often lost in translation. For example, Wang and Robertson (2008) state that point configuration should not be based on treating a symptom or illness but considered within a more holistic context and what the specific effects are on the transformation of Qi. Maciocia (2008) recommends different acupuncture point configuration that correlates with the underlying pattern rather than the actual disease, such as PD. For example, using different acupuncture points for the underlying pattern of Kidney Yin deficiency and a different set of acupuncture points for the other patterns such as Liver-Yang rising, that all cause Internal Wind. This recommendation seems a more balanced approach for point selection in future RCTs; avoiding the extremes of standardising point selection based on the Western classification of PD, and the other extreme of individualisation which uses a myriad of factors dependent upon the CM training, experience and biases of the acupuncturist.
These factors within acupuncture can take many forms. For example, Maciocia (2008) advises practitioners when treating PD to use a dispersing needle technique for points that extinguish Wind and a tonifying needle technique for points that nourish Liver-Blood or Yin. The Su Wen and Ling Shu explain needle techniques that including the depth of insertion, direction when rotating the needle, insertion time of the needle dependent upon the exhalation and inhalation of the patient and whether to close or leave open the hole after finishing needling (Unschuld, 2003; Unschuld, 2016). The significance of needle technique finds further support by a recent study that concluded that acupuncture sensation and pain threshold increase depend upon the depth and rotation of the needle (Choi, Lee, Moon and Cho, 2013). Maciocia (2015) states that Da Zhu (Du 14) can have ‘opposite effects’ dependent on the needle technique and the directional rotation of the needle. None of the studies in this CLR noted the needle technique employed other than reporting the depth of needling and the De Qi response (See appendix 2).
In addition to the variations in acupuncture point selection and needle technique, the trials also showed varying treatment frequency, needle retention time, electrical stimulation frequency, needle depths, needle width and the number of needles used (See appendix 2). The number of variants in the included studies, highlights the lack of consensus on a standardised treatment for treating motor related symptoms of PD. This lack of standardisation may be due to a lack of coherence in the application of CM theory or a symptom of the individualisation of acupuncture treatments. Moreover, it may lend support to a new paradigm of assessing the effects of acupuncture on diseases, such as PD. MacDonald (2019) argues that the issues with sham acupuncture are insurmountable and that the question of efficacy of interventions is misguided. MacDonald (2019) suggests contrasting two or more therapies in an open pragmatic trial; comparing them in terms of effectiveness rather than efficacy; as well as safety and cost-effectiveness. The effectiveness of two interventions running in parallel in ordinary day-to-day circumstances would be hard to quantify accurately without external and internal influences affecting the quality of the results. And whilst an extensive examination of this approach is beyond the scope of this paper; in the context of this CLR it should be acknowledged that this would allow the practitioner more flexibility to treat the underlying patterns that are manifesting with motor related symptoms of PD, rather than using a standardised point configuration approach. However, PD is difficult to diagnose and often only confirmed when the patient responds to PD medications such as Levodopa (Suchowersky et al., 2006). Therefore, one of the issues with open pragmatic trials contrasting acupuncture with medication such as Levodopa, is finding participants who have been diagnosed with PD and have not yet taken PD medication.
5. Conclusion
The weight of evidence to successfully treat motor related symptoms of PD with acupuncture is growing. However, the methodologies of many of recent trials is of poor or average quality with no adequate control to mitigate the placebo effect, undermining the hypothesis of the efficacy of acupuncture in alleviating symptoms of PD (Lam et al., 2008). Cho et al. (2017) highlighted the value of follow-up data, showing that the therapeutic effects of sham acupuncture were not sustainable in the long term compared with real acupuncture. The long-term effects of sham acupuncture need to be studied to determine whether they are ethically sound as a placebo control.
The efficacy of different acupuncture points in treating the symptoms of motor related PD was measured through averaging the P-values from the included trials. The average P-value of different acupuncture points was noteworthy, however any claim of efficacy of one acupuncture point over another in treating PD would be unsubstantiated due to the variations in design and methodology of the studies.
Proposing new models, such as open pragmatic trials (MacDonald, 2019) to measure acupuncture’s effectiveness in treating PD is unlikely to convince the Western scientific community; which takes RCTs as the established gold standard for the efficacy of interventions (Schulz, Altman and Moher, 2010). Therefore, a middle path between standardisation and individualisation, may be to find a consensus on acupuncture point selections that treat the underlying patterns of Internal Wind, rather than PD itself. The STRICTA checklist could be enhanced to include the underlying pattern of the patient suffering from PD and then the acupuncture points would be selected, based on the consensus within the acupuncture community, to treat that pattern. Though other factors in formulating acupuncture point configurations would be ignored, it would resolve the inconsistencies in acupuncture point selection. Therefore, future research may be to look at the efficacy of acupuncture point configurations when treating individual patterns that underlie PD and then apply those configurations in larger, placebo controlled trials with rigorous methods of randomization, blinding and concealed allocation.
References
Ariadna, R. and Benjamin, D., 2014. Alpha-Synuclein Spreading in Parkinson’s Disease. [online] Frontiers in Neuroanatomy. Available at: <https://www.frontiersin.org/articles/10.3389/fnana.2014.00159/full> [Accessed 18 April 2020].
Alexander, G., 2004. Biology of Parkinson’s Disease: Pathogenesis and Pathophysiology of a Multisystem Neurodegenerative Disorder. [online] Available at: <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181806/> [Accessed 9 April 2020].
Altman DG, Hammerschlag R, Li Y, MacPherson H, Moher D, White A, Wu T (on behalf of the STRICTA Revision Group) (2010) Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT Statement available at: http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000261 (accessed 19/04/19).
Aosaki, T., Miura, M., Suzuki, T., Nishimura, K. and Masuda, M., 2010. Acetylcholine-Dopamine Balance Hypothesis in The Striatum: An Update. [online] Wiley Online Library. Available at: <https://onlinelibrary.wiley.com/doi/10.1111/j.1447-0594.2010.00588.x> [Accessed 14 May 2020].
Bassetto, J., Zeigelboim, B., Jurkiewicz, A. and Klagenberg, K., 2008. Neurotological Findings in Patients With Parkinson’s Disease. [online] Science Direct. Available at: <https://www.sciencedirect.com/science/article/pii/S180886941530567X?via%3Dihub> [Accessed 13 May 2020].
Brim, R. and Miller, F., 2013. The Potential Benefit of The Placebo Effect in Sham-Controlled Trials: Implications for Risk-Benefit Assessments And Informed Consent. [online] BMJ. Available at: <https://jme.bmj.com/content/medethics/39/11/703.full.pdf> [Accessed 20 May 2020].
Chen, F., Chang, C., Shiu, J., Chiu, J., Wu, T., Yang, J., Kung, Y., Chen, F., Chern, C. and Hwang, S. (2015). A Clinical Study of Integrating Acupuncture and Western Medicine in Treating Patients with Parkinson’s Disease. The American Journal of Chinese Medicine, 43(03), pp.407-23.
Cho, S., Shim, S., Rhee, H., Park, H., Jung, W., Moon, S., Park, J., Ko, C., Cho, K. and Park, S. (2012). Effectiveness of acupuncture and bee venom acupuncture in idiopathic Parkinson’s disease. Parkinsonism & Related Disorders, 18(8), pp.948-52
Choi, Y., Lee, J., Moon, W. and Cho, S., 2013. Does the Effect Of Acupuncture Depend On Needling Sensation And Manipulation? [online] Science Direct. Available at: <https://www.sciencedirect.com/science/article/abs/pii/S0965229912001756> [Accessed 19 May 2020].
Dashtdar, M., Dashtdar, M. R., Dashtdar, B., Kardi, K., & Shirazi, M. K. (2016). The Concept of Wind in Traditional Chinese Medicine. Journal of pharmacopuncture, 19(4), 293–302. https://doi.org/10.3831/KPI.2016.19.030
Deadman, P., Al-Khafaji, M. and Baker, K., 2016. A Manual of Acupuncture. East Sussex, England: Journal of Chinese Medicine Publications.
De la Fuente-Fernandez, R. and Stoessl, J., 2002. Expectation and Dopamine Release: Mechanism of The Placebo Effect In Parkinson’s Disease. [online] Trends in Neuroscience. Available at: <https://pubmed.ncbi.nlm.nih.gov/12086748/> [Accessed 11 May 2020].
Dong, Z., Zhang, Z. and Román, G. (2006). Early Descriptions of Parkinson Disease in Ancient China. [online] ResearchGate. Available at: https://www.researchgate.net/publication/7097759_Early_Descriptions_of_Parkinson_Disease_in_Ancient_China [Accessed 6 Apr. 2019].
Doo, K., Lee, J., Cho, S., Jung, W., Moon, S., Park, J., Ko, C., Kim, H., Park, H. and Park, S. (2015). A Prospective Open-Label Study of Combined Treatment for Idiopathic Parkinson’s Disease Using Acupuncture and Bee Venom Acupuncture as an Adjunctive Treatment. The Journal of Alternative and Complementary Medicine, 21(10), pp.598-603.
Fan, J., Hiroki, N., Zhongren, S., Tetsuya, A., Yuhuai, G., Hongna, Y. and Tiansong, Y. (2018). Evidence for the Use of Acupuncture in Treating Parkinson’s Disease: Update of Information from the Past 5 Years, a Mini Review of the Literature. [online] Frontiers in Neurology. Available at: https://www.frontiersin.org/articles/10.3389/fneur.2018.00596/full [Accessed 5 Apr. 2019].
Ferry, P., Johnson, M. and Wallis, P., 2002. Use of Complementary Therapies and Non-Prescribed Medication in Patients with Parkinson’s Disease. [online] PMC. Available at: <https://pmj.bmj.com/content/postgradmedj/78/924/612.full.pdf> [Accessed 20 April 2020].
Ghaffari, B. and Kluger, B., 2014. Mechanisms for Alternative Treatments In Parkinson’s Disease: Acupuncture, Tai Chi, And Other Treatments. [online] PubMed. Available at: <https://www.ncbi.nlm.nih.gov/pubmed/24760476> [Accessed 10 May 2020].
Goetz, C. G., Fahn, S., Martinez-Martin, P., Poewe, W., Sampaio, C., Stebbins, G. T., Stern, M. B., Tilley, B. C., Dodel, R., Dubois, B., Holloway, R., Jankovic, J., Kulisevsky, J., Lang, A. E., Lees, A., Leurgans, S., LeWitt, P. A., Nyenhuis, D., Olanow, C. W., Rascol, O., Schrag, A., Teresi, J. A., Van Hilten, J. J. and LaPelle, N. (2008) Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Process, format, and clinimetric testing plan. Pubmed. Available at http://onlinelibrary.wiley.com/doi/10.1002/mds.22340/full [Last accessed 03/03/2018]
Golding, R. (2008). The complete stems and branches. Edinburgh: Churchill Livingstone/Elsevier.
Kim, H., 2015. Statistical Notes for Clinical Researchers: Type I And Type II Errors In Statistical Decision. [online] PMC. Available at: <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4534731/> [Accessed 13 May 2020].
Kluger, B. M., Rakowski, D., Christian, M., Cedar, D., Wong, B., Crawford, J., Garvan, C. (2016). Randomized, controlled trial of acupuncture for fatigue in Parkinson’s Disease. Movement Disorders, 31, 1027-32.
(accessed 01/04/2019)
Lam, Y., Kum, W., Durairajan, S., Lu, J., Man, S., Xu, M., Zhang, X., Huang, X. and Li, M., 2008. Efficacy and Safety of Acupuncture for Idiopathic Parkinson’s Disease: A Systematic Review. The Journal of Alternative and Complementary Medicine, 14(6), pp.663-671.
Lee, M., Shin, B., Kong, J. and Ernst, E., 2008. Effectiveness of Acupuncture for Parkinson’s Disease: A Systematic Review. [online] Wiley Online Library. Available at: <https://onlinelibrary.wiley.com/doi/abs/10.1002/mds.21993> [Accessed 1 May 2020].
Lee, S. and Lim, S. (2017). Clinical effectiveness of acupuncture on Parkinson disease: A PRISMA-compliant systematic review and meta-analysis. [online] Wolters Kluwer Health, Inc. Available at: https://journals.lww.com/md-journal/Fulltext/2017/01200/Clinical_effectiveness_of_acupuncture_on_Parkinson.14.aspx [Accessed 6 Apr. 2019].
Lee, J., Napadow, V., Kim, J., Lee, S., Choi, W., Kaptchuk, T. and Park, K., 2014. Phantom Acupuncture: Dissociating Somatosensory and Cognitive/Affective Components of Acupuncture Stimulation with a Novel Form of Placebo Acupuncture. PLoS ONE, 9(8), p.e104582.
Lidstone, Sarah C. PhD; Michael Schulzer, MD, PhD; Katherine Dinelle, MSc; Edwin Mak, BSc; Vesna Sossi, PhD; Thomas J. Ruth, PhD; Raul de la Fuente-Fernández, MD; Anthony G. Phillips, PhD; A. Jon Stoessl, MD. (2010) Effects of Expectation on Placebo-Induced Dopamine Release in Parkinson Disease. Arch Gen Psychiatry. 2010;67(8):857–865. doi:10.1001/archgenpsychiatry.2010.88
Linde, K, Witt, C.M., Streng, A., Weidenhammer, W., Wagenpfeil, S., Brinkhaus, B., Willich, S.N., Melchart, D. (2007) The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Available at https://www.ncbi.nlm.nih.gov/pubmed/17257756 [accessed Feb 24, 2019].
MacDonald, J., 2019. Why Randomised Placebo-Controlled Trials Are Inappropriate for Acupuncture Research – General Discussion – JCM Article Archive. [online] Journalofchinesemedicine.com. Available at: <https://www.journalofchinesemedicine.com/why-randomised-placebo-controlled-trials-are-inappropriate-for-acupuncture-research.html> [Accessed 25 April 2020].
Maciocia, G. (2006). The Channels of Acupuncture: Clinical Use of the Secondary Channels and Eight Extraordinary Vessels. Edinburgh: Churchill Livingstone.
Maciocia, G. (2008). The Practice of Chinese medicine: The treatment of diseases with acupuncture and Chinese herbs. 2nd ed. Churchill Livingstone; London
Maciocia, G. (2015) The Foundations of Chinese Medicine 2nd ed. Churchill Livingstone; London
Matsubara, T., Shimo, K., Nishihara, M., Sato, J., Ushida, T., Shiro, Y. and Arai, Y. (2011). Comparative Effects of Acupressure at Local and Distal Acupuncture Points on Pain Conditions and Autonomic Function in Females with Chronic Neck Pain. [online] NCBI. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2952311/ [Accessed 8 Apr. 2019].
NHS, 2016. Parkinson’s Disease. [online] nhs.uk. Available at: <https://www.nhs.uk/conditions/parkinsons-disease/> [Accessed 22 January 2020].
Pagano, G., Ferrara, N., Brooks, D. J., & Pavese, N. (2016). Age at onset and Parkinson disease phenotype. Neurology, 86(15), 1400–1407. https://doi.org/10.1212/WNL.0000000000002461
Parkinson’s Foundation. (2019). Causes Parkinson’s Disease. [online] Available at: https://www.parkinson.org/Understanding-Parkinsons/Causes?_ga=2.64782959.1948268554.1555682789-1524377684.1555414469 [Accessed 4 Apr. 2019].
Parkinsons UK (2018). Complementary Therapies and Parkinsons. [online] Available at: https://www.parkinsons.org.uk/information-and-support/ complementary therapies [Accessed 19 March 2019].
Ramsden, D., Parsons, R., Waring, R. and Ho, S., 2001. The Aetiology of Idiopathic Parkinson’s Disease. [online] PubMed Central (PMC). Available at: <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1187126/> [Accessed 9 April 2020].
Schulz, K., Altman, D. and Moher, D., 2010. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ, [online] 11(1). Available at: <https://www.bmj.com/content/340/bmj.c332>.
Suchowersky, O., Reich, S., Perlmutter, J., Zesiewicz, T., Gronseth, G. and Weiner, W., 2006. Practice Parameter: Diagnosis and prognosis of new onset Parkinson disease (an evidence-based review). Neurology, [online] 66(7), pp.968-975. Available at: <https://pubmed.ncbi.nlm.nih.gov/16606907/> [Accessed 21 May 2020].
Sidransky, E. and Lopez, G. (2014). The link between the GBA gene and Parkinsonism. [online] NCBI. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4141416/ [Accessed 13 Apr. 2019].
Stephenson, C. (2017). Acupuncturists guide to conventional medicine, second edition. 2nd ed. Singing Dragon.
Stoker, T. and Greenland, J., 2018. Parkinson’S Disease: Pathogenesis and Clinical Aspects – Pubmed – NCBI. [online] Ncbi.nlm.nih.gov. Available at: <https://www.ncbi.nlm.nih.gov/pubmed/30702835> [Accessed 18 April 2020].
Thanvi, B. and Lo, T. (2003). Long term motor complications of levodopa: clinical features, mechanisms, and management strategies. [online] BMJ Journals. Available at: https://pmj.bmj.com/content/80/946/452 [Accessed 9 Apr. 2019].
Toosizadeh, N., Lei, H., Schwenk, M., Sherman, S., Sternberg, E., Mohler, J. and Najafi, B. (2015). Does Integrative Medicine Enhance Balance in Aging Adults? Proof of Concept for the Benefit of Electroacupuncture Therapy in Parkinson’s Disease. Gerontology, 61(1), pp.3-14.
Unschuld, P., 2003. Huang Di Nei Jing Su Wen. Berkeley, Calif.: University of California Press.
Unschuld, P. (2016). Huang Di Nei Jing Ling Shu. Berkeley: University of California Press.
Unschuld, P. (2016) Nan Jing. 2nd ed. Berkeley: University of California Press.
Van Kervel, P. (2012). Celestial stems & terrestrial branches. Kockengen: Lán Dì Press.
Varanese, S., Birnbaum, Z., Rossi, R. and Di Rocco, A. (2011). Treatment of Advanced Parkinson’s Disease. [online] ResearchGate. Available at: https://www.researchgate.net/publication/49845726_Treatment_of_Advanced_Parkinson’s_Disease [Accessed 1 Apr. 2019].
Vidgen, B. and Yasseri, T. (2016). P-Values: Misunderstood and Misused. [online] Frontiers in Physics. Available at: <https://www.frontiersin.org/articles/10.3389/fphy.2016.00006/full> [Accessed 18 May 2020].
Wang, JY. and Robertson, J. (2008) Applied Channel Theory in Chinese Medicine.
Seattle: Eastland Press.
Were, H. (2018). Can Acupuncture Improve the Quality of Life for People Suffering from Parkinson’s Disease? [online] The European Journal of Oriental Medicine. Available at: http://www.ejom-archive.co.uk/volume-9-number-2/articles/can-acupuncture-improve-the-quality-of-life-for-people-suffering-from-parkinsons-disease.html [Accessed 4 Apr. 2019].
Whitlock, M., 2005. Combining Probability from Independent Tests: The Weighted Z-Method Is Superior To Fisher’s Approach. [online] Wiley Online Library. Available at: <https://onlinelibrary.wiley.com/doi/full/10.1111/j.1420-9101.2005.00917.x> [Accessed 14 May 2020].
Yeo, S., Van den Noort, M., Bosch, P. and Lim, S. (2019). A study of the effects of 8-week acupuncture treatment on patients with Parkinson’s disease. [online] NCBI. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6320216/ [Accessed 7 Apr. 2019].
Bibliography
Chen, F., Chang, C., Shiu, J., Chiu, J., Chernyand, C. and Hwang, S. (2015) A Clinical Study of Integrating Acupuncture and Western Medicine in Treating Patients with Parkinson’s Disease. The American Journal of Chinese Medicine Available at https://www.researchgate.net/publication/276362892_A_Clinical_Study_of_Integrating_Acupuncture_and_Western_Medicine_in_Treating_Patients_with_Parkinson’s_Disease/overview [accessed Feb 24 2019].
Chinesemedicinetraveller.com. (2020). Chinese Medicine Traveller » Blog Archive » Acupuncture Slows the Progression of Parkinson’s. [online] Available at: https://chinesemedicinetraveller.com/?article=acupuncture-slows-the-progression-of-parkinsons [Accessed 9 Feb. 2020].
Cochrane Bias Methods Group (2017) The Cochrane Risk of Bias Tool available at: http://methods.cochrane.org/bias/assessing-risk-bias-included-studies (accessed 19/04/19).
CONSORT (Consolidated Standards of Reporting Trials) checklist (2010)
Critical Appraisal Skills Programme (2018) CASP Randomised Controlled Trial Checklist. Available at: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Randomised-Controlled-Trial-Checklist-2018.pdf [Accessed 6 Apr. 2019].
Jang, J., Kim, H., Jung, I. and Yoo, H. (2018). Acupuncture for improving gait disturbance in Parkinson’s disease: A study protocol for a pilot randomized controlled trial. [online] ScienceDirect. Available at: https://www.sciencedirect.com/science/article/pii/S1876382018300878?via%3Dihub [Accessed 3 Apr. 2019].
Lei, H., Toosizadeh, N., Schwenk, M., Sherman, S., Karp, S., Parvaneh, S., Esternberg, S., Najafi, B. (2014). Objective Assessment of Electroacupuncture Benefit for Improving Balance and Gait in Patients with Parkinson’s Disease. Neurology, Apr 2014, 82 (10 Supplement) P3.074.
Lei, H., Toosizadeh, N., Schwenk, M., Sherman, S., Karp, S., Sternberg, E. and Najafi, B. (2016). A Pilot Clinical Trial to Objectively Assess the Efficacy of Electroacupuncture on Gait in Patients with Parkinson’s Disease Using Body Worn Sensors. PLOS ONE, 11(5).
Li, L.H., Zhang H. F., Cao, L., Yin J.Q., Wang, F. (2016). Efficacy of Thick Needling at Shenzu Acupoint in Treating Parkinson’s Disease. Oxidation Communications 39, No 4-IV, 4218-24.
Ostrovsky, D. and Ehrlich, A. (2019). Bee Venom Acupuncture in Addition to Anti-Parkinsonian Medications May Improve Activities of Daily Living and Motor Symptoms More Than Medication Alone in Idiopathic Parkinson’s Disease. [online] ScienceDirect. Available at: https://www.sciencedirect.com/science/article/pii/S1550830718304397?via%3Dihub [Accessed 15 Apr. 2019].
Schliessbach, J., van der Klift, E., Arendt-Nielsen, L., Curatolo, M. and Streitberger, K., 2011. The Effect of Brief Electrical and Manual Acupuncture Stimulation on Mechanical Experimental Pain. [online] Oxford Academic. Available at: <https://academic.oup.com/painmedicine/article/12/2/268/1855465> [Accessed 8 May 2020].
Shulman, L., Wen, X., Weiner, W., Bateman, D., Minagar, A., Duncan, R. and Konefal, J., 2002. Acupuncture Therapy for The Symptoms Of Parkinson’s Disease. [online] Wiley Online Library. Available at: <https://onlinelibrary.wiley.com/doi/abs/10.1002/mds.10134> [Accessed 14 May 2020].
Snow, B. (2003) Objective measures for the progression of Parkinson’s disease
Journal of Neurology, Neurosurgery & Psychiatry. Last accessed 02/03/2019 available at http://jnnp.bmj.com/content/74/3/287.
Toosizadeh, N., Lei, H., Schwenk, M., Sherman, S., Esternberg, E. and Najafi, B. (2014). Effectiveness of Electroacupuncture Therapy in Improving Gait and Balance in People with Parkinson’s Disease. The Journal of Alternative and Complementary Medicine, 20(5), pp. A45-A45.
Appendices
Appendix 1 – Databases Searched
Cochrane Library | 65 |
PUBMED | 18 |
Greenwich E-Library | 101 |
Trip Database | 19 |
Google Scholar | 41 |
Science Direct | 46 |
Library Handsearch | 3 |
EJOM | 1 |
JCM | 1 |
Wiley Online Library | 14 |
